Ahead of the Curve: Region 1’s Public Health Workforce Plan
A conversation between Erin Braasch & Sarah Tennyson
11/13/23
Erin Braasch: Good morning, Sarah.
Sarah Tennyson: Hey, Erin. Good morning.
Erin Braasch: I’m so glad to be able to spend this time talking with you about a project we got to do together. So, everybody watching: I’m Erin Braasch and the executive director for WNC Health Network. We had the pleasure of supporting Public Health Region One in developing their public health workforce plan. We know that it’s been put to use and there’s been some interest across the state in how you did this and so, just wanted to spend some time today talking about that project. Before we launch, Sarah, tell us a little bit about who you are and your role with Public Health Region One and the kinds of things you do day-to-day.
Sarah Tennyson: My name is Sarah Tennyson, I’m the Workforce Development Director for Region One Health Departments. The region one health departments go over from Cherokee County to Haywood & Transylvania, so it’s eight counties in the far west. As the Workforce Development Director, I’m technical assistant to each of the health departments, especially when it comes to recruiting and retaining staff. 46% of our public health staff left after COVID [nationwide]. And so this position was created to help fill those gaps of figuring out ways to support our existing workforce and recruit our workforce coming into public health.
Erin Braasch: So shifting to talk about this specific project that we worked on together, can you give us a little bit of background about it?
Sarah Tennyson: The way that this project worked was the health departments received a grant; it was the ARPA grant – the American Rescue Plan Act funding. After COVID happened, like I was mentioning, there was an exodus of the public health staff. With this funding, it was really to help us fill some gaps in the foundational capabilities of public health. And so the way that we did this is there was quite a bit of data that was collected. We interviewed staff for health departments across the state to see what do you need in your position, what kind of training technical assistance support do you need in your day-to-day life in the health department? So we got a lot of information back from our staff to figure out ways to help support them. We heard directly from the people that are most affected.
But as it happens with public health money, oftentimes we get the funding [but] we have such a short turnaround of how we’re going to spend that money. And so we have to make some very quick decisions. And so this is just kind of how we operate in public health. What we thought as the Region One Health Departments is that we have a limited amount of money, we had a limited timeframe. And so we needed to be very smart with our money in terms of making longer, sustainable impacts. We had this money, we wanted to make it last so what we wanted to do was to come up with a strategic plan to help guide us over the next five years, to make sure we were making informed decisions and the smartest decisions for the region. And so we decided that a strategic plan would be the way to help us get there.
We’ve worked with the [WNC] Health Network over the years to do things like this and my experience with the Health Network is that when we have a complex issue, we have a variety of different agencies with different agendas, different priorities, different capacity, is that we needed to be able to bring an external partner in and so the Health Network was a good fit for this kind of thing. To come in, bring all these different diverse people, personalities, agendas together, in a short amount of time to be able to synthesize a plan for us to be able to follow over the next five years. And so that was what got us to the point to want to develop a formal plan.
Erin Braasch: And who remind us who was all at the table? When you say “we,” who was involved in coming up with a plan.
Sarah Tennyson: It was the Region One Health Departments, and so it was each of the health directors from the county so that would be Cherokee, Clay, Graham, Macon, Swain, Jackson, Haywood, and Transylvania and myself. We think about it like, Oh, I couldn’t possibly facilitate this. But what I find so nice is having kind of an external neutral party that comes in because that helps me as the director of the program participate in the process as well, and also to kind of have that external support. So it’s kind of a neutral party that’s able to come in to help facilitate the process. So that I find is really nice to have someone like you all come in to do that.
Erin Braasch: Thank you, Sarah. We certainly appreciate the depth in which you participate. One of our values when we provide this kind of support is co-design so that we know that we’re uniquely meeting the need. So you, you know you had a very clear vision of what needed to happen and it was exciting.
Sarah Tennyson: I just wanted to add as I was thinking about the answer to this question ahead of time, and part of it is, Emily Kujawa was the facilitator along with you, which was really nice, but Emily and I before that session, we had many many meetings ahead of time and so I think that’s really important distinction. During that meeting I was the neutral person but ahead of time, her and I really did codesign that together — the process, the questions, the product. And so I really appreciate that aspect because I was right there with the process ahead of time, during, and after but then the day of it I could try to step back. And so that was just an important distinction. So I appreciate you bringing that up.
Erin Braasch: So now that this project happened a good while ago, what’s going on with the plan?
Sarah Tennyson: Well, it’s been really, really nice because, you know, in public health, oftentimes, funding is what we sometimes call braided funding, because it’s never straightforward. It’s rarely straightforward. Oftentimes, we have an issue or something we’re trying to address and we have to figure out ways to make it work. One thing I will mention about the Regional Health Departments is they’re very resilient. They’re used to working together. They’re used to… taking a small amount of money, expanding it, finding other ways to fund certain project to build the capacity for something and so what we’ve been able to do is take that plan and approach different funders and apply for different grant funding streams, where we prioritize certain pieces of this workforce plan. So I can apply to a certain funder for something that would fit appropriately what that funder is looking for where we’re also getting other funds for the state. We can kind of piece together what we’re able to fund from different sources. And so, I’ve used that plan multiple times over the last year and it’s so nice to just have this nice, tangible product that really supports my work and leveraging additional funds. And so it helps me be successful for the region. It’s really nice to have that.
Erin Braasch: You mentioned the state and I’m curious what the response has been in other parts of the state to your plan or from the state itself.
Sarah Tennyson: We’ve gotten a lot of really positive feedback from other regions in the state and the reason why is because we knew that these funds would end in May of 2024 and we’re prepared for that. So we did this plan last year kind of anticipating we would have a year left. I think when grants wrap up a lot of times, it’s like, oh, sustainability, what are we going to do next? And so I kind of feel like our region was ahead of the curve, because we had already gone through this process. We already had these pieces in place. And so across the state I had been sharing about our process to my counterparts and other regions in the state. And so they were very curious and would reach out to me to say, How did you do this? What questions did you ask, what was your process? Can we see the plan? And so I got a lot of really nice feedback from other regions across the state, wanting to replicate or get some feedback on how they could do something similar.
Erin Braasch: Great, Sarah. We certainly enjoyed working with you on this project. Thank you for being a great partner with us.
Sarah Tennyson: Yeah, it was awesome. Thank you so much for helping us, it’s been really really wonderful.
To learn more about Region 1 Public Health Workforce, email Sarah Tennyson at sarah.tennyson@transylvaniacounty.org. To learn more about WNC Health Network’s services that can support your work, visit here.















 Carol Pitts with the
Carol Pitts with the 
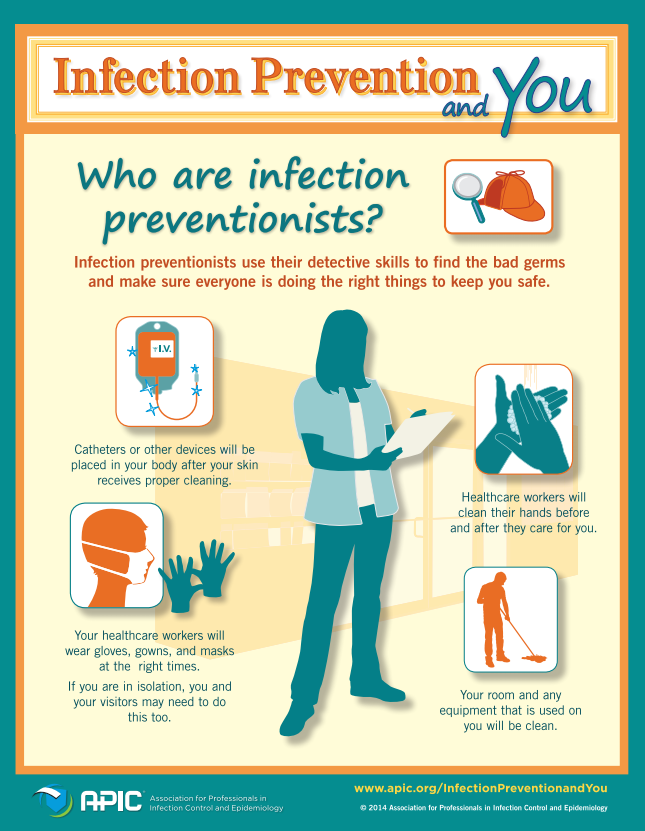



 Motivational interviewing (MI) is an evidence-based approach to behavior change that is grounded in a respectful conversation between provider and patient to identify a patient’s readiness for change, and that helps the patient come up with ideas about how they can strengthen their motivation to change. Making MI the foundation of anticipatory guidance assures that providers listen to the concerns of parents and children, understand their ambivalence to change, and support their ideas about change and what they think would work. In a dental setting, MI shifts the conversation from a one-way monologue about brushing their teeth and cutting down on sugar to a conversation about the parent and child’s experiences, challenges, and ideas about what needs to change and how the provider can support them in making the needed changes.
Motivational interviewing (MI) is an evidence-based approach to behavior change that is grounded in a respectful conversation between provider and patient to identify a patient’s readiness for change, and that helps the patient come up with ideas about how they can strengthen their motivation to change. Making MI the foundation of anticipatory guidance assures that providers listen to the concerns of parents and children, understand their ambivalence to change, and support their ideas about change and what they think would work. In a dental setting, MI shifts the conversation from a one-way monologue about brushing their teeth and cutting down on sugar to a conversation about the parent and child’s experiences, challenges, and ideas about what needs to change and how the provider can support them in making the needed changes.